Thuma Mina moment as professionals step forward to address the COVID-19 crisis
Drickus Maartens • June 5, 2020
Blueprints for Cecilia Makiwane Gallagher Critical Care Hospital ready and waiting
Eighty professionals have stepped forward as volunteers to bring one of SA’s most ambitious COVID-19 critical care projects to fruition.
The team comprising actuaries, engineers, doctors, architects, project specialists and others have been toiling behind the scenes since early March to put together blueprints for a dedicated, state-of-the-art, fully equipped and staffed, emergency and critical care COVID-19 testing and treatment hospital. The group also includes individuals who have been involved in the integrated building and commissioning of private and public hospitals over the past 40 years and have volunteered their expertise and time as they are, without exception, committed to saving lives.
The projected medical facility will be named the Cecilia Makiwane Gallagher Critical Care Hospital, in recognition of South Africa and the continent’s first black registered professional nurse, who qualified in 1908, and went on to become a South African healthcare pioneer and human rights campaigner. It will be equipped up to high care or critical care specifications.
The hospital, which has been earmarked for development in Midrand, is geared to operate as a dedicated critical care facility for COVID-19 patients, will initially have 524 beds and is designed to be upscaled to 1 178 beds, without the need to build a second duplicate infrastructure.
A heartfelt calling in a time of need
The project is the brainchild of Dr Johan Pretorius, a medical doctor and a director of the not-for-profit Universal Healthcare Foundation, who shares a heartfelt calling and mission with the group of like-minded professionals who are devoting their time to the project pro-bono.
Commenting on the initiative, Dr Pretorius said that actuaries, who are part of the team, have provided detailed analyses on the pandemic, including the experiences of other countries, and the available infrastructure in South Africa. “We have carefully interrogated projections from all experts, nationally and internationally, and our own actuaries concur with the most recent projections of loss of life and shortage of ICU beds that lie ahead in the months to come, as presented by Dr Sheetal Silal of the Department of Statistical Sciences at the University of Cape Town (UCT). All indications suggest that there are dire days ahead in the fight against COVID-19, unless South Africans band together to take swift and drastic action in preparing for the peak of the pandemic.
“Based on our projections, we are certain that we are going to run out of critical care beds in South Africa in the coming months. The Cecilia Makiwane Gallagher Critical Care Hospital, which will add more critical care beds for really ill COVID-19 patients requiring hospitalisation, is in our view of vital importance and extremely urgent. Seriously ill hospitalised patients require uninterrupted high flow oxygen, and may require respiratory support, either with continuous positive pressure (CPAP) machines, or in the worst of cases, full intubation and ventilation in a critical care facility, of which we have a dire shortage.
As we have seen from the Cape Town experience, time is of the essence. It is therefore imperative that this additional facility is operational by the time South Africa reaches the peak of the pandemic, which based on current estimates, would be in July/August 2020,” he cautions.
“It is the aim of the Universal Foundation to provide a meaningful solution, which we envisage will help to reduce the burden on South Africa’s healthcare infrastructure for patients located in the Gauteng area, who are very ill and require hospitalisation and specialised care.
“After having discussed our proposal with the Acting Director General: Health, at the end of March 2020, he appointed me to the Infrastructure Office of the National Department of Health so that we could immediately commence with our work,” he explains. “We have had a number of positive and collaborative interactions to establish this facility as a private-public partnership, but unfortunately no decisions have been forthcoming yet and we cannot proceed to build a facility without the necessary approval.”
No ordinary project
According to Dr Pretorius, the Cecilia Makiwane Gallagher Critical Care Hospital is no ordinary project.
“We believe this facility can potentially save thousands of lives during the pandemic. That is why we have put together a plan to operate a sophisticated hospital facility with a dedicated critical care capability, and with flexibility to scale up or down the number of beds as required.
“We anticipate that it will operate for seven months during the most intense part of the pandemic, with a month to set up the facility beforehand and a month to decommission the hospital at the end after a period of some nine months.
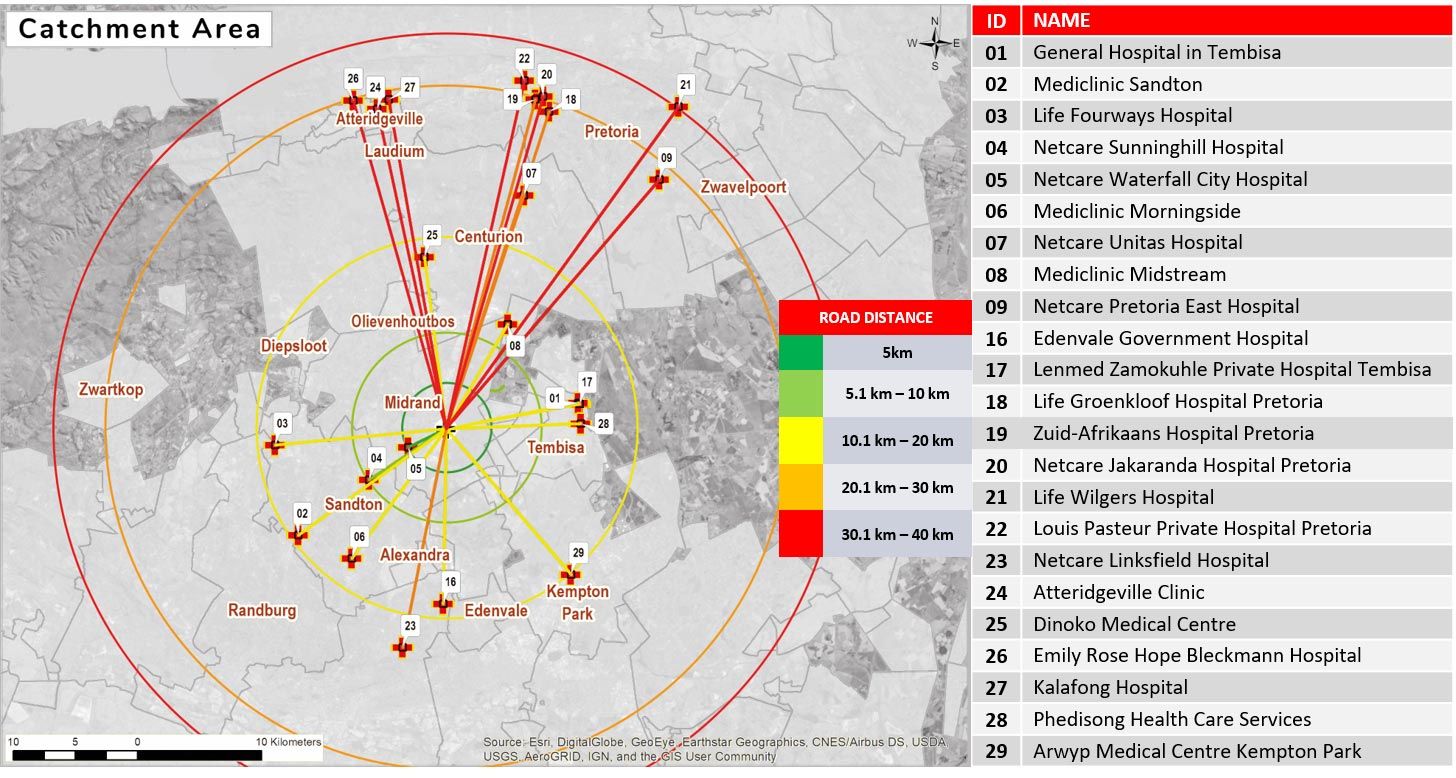
The Foundation has looked at other ways to contain costs, including building an emergency tent hospital. Even the repurposing of existing, but abandoned buildings was considered, however the location of these facilities was not as central, easily accessible and with required infrastructure already in place, as the proposed location – Gallagher Convention Centre. Midrand offers an ideal location in the centre of Gauteng.
A South African version of the UK’s Nightingale Hospitals
Dr Pretorius says that the hospital can be built in approximately four weeks, following a similar model to the Nightingale Hospitals in the United Kingdom, but modified for the South African context, before being decommissioned at the end of the period. “We operate in a very different environment to the UK and other first world environments, and have to operate with limited resources and a shortage of highly trained medical and nursing professionals who will be essential for a facility such as this.”
Once decommissioned, all capital and reusable goods will be donated to the National Department of Health for redeployment within the public sector to assist the Government in their plans and objectives for National Health Insurance.
“This temporary Critical Care Hospital will complement the good work done by Government on the current COVID-19 pandemic with other facilities such as Nasrec. We also submit that since Nasrec is already a large facility, the central location of the proposed hospital is very important and has therefore been well researched to ensure that it has optimal accessibility, strategically complementing the capacity available in this densely populated, key economic province,” notes Dr Pretorius.
Funding of the hospital
While negotiations are ongoing, it is proposed that the hospital could be funded as part of a private-public partnership between Government and the Universal Healthcare Foundation and its fundraising efforts in the private sector. The Universal Foundation
will also work closely with Business South Africa, the private and public sectors, and the Solidarity Fund.